Prediction model reveals new characteristics that may affect risk

Cleveland Clinic researchers have developed the world’s first risk prediction model for healthcare providers to forecast an individual patient’s likelihood of testing positive for COVID-19 as well as their outcomes from the disease.
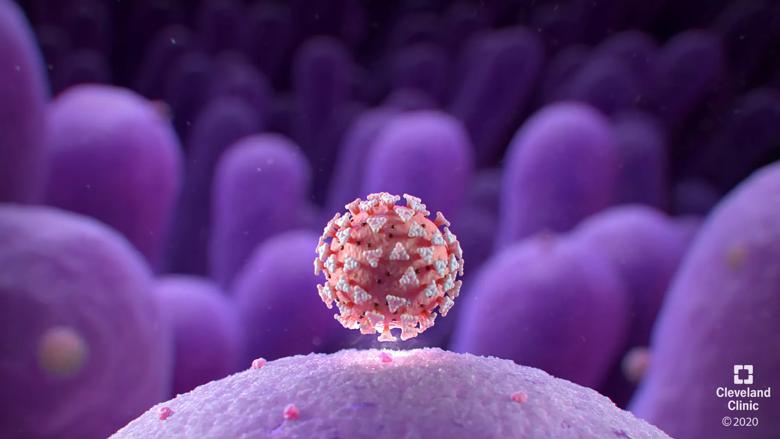
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/813e0a96-5ce2-4254-acd4-7608e9555aa8/cleveland-clinic-covid19-illustration-logo-3-scaled_jpg)
According a new studypublished in CHEST, the risk prediction model (called a nomogram) shows the relevance of age, race, gender, socioeconomic status, vaccination history and current medications in COVID-19 risk. The risk calculator is a new tool for healthcare providers to aid them in predicting patient risk and tailoring decision-making about care. It provides a more scientific approach to testing which is important for the healthcare community which has faced increased demand for testing and limited resources.
“The ability to accurately predict whether or not a patient is likely to test positive for COVID-19, as well as potential outcomes including disease severity and hospitalization, will be paramount in effectively managing our resources and triaging care,” said Lara Jehi, M.D., Cleveland Clinic’s Chief Research Information Officer and corresponding author on the study. “As we continue to battle this pandemic and prepare for a potential second wave, understanding a person’s risk is the first step in potential care and treatment planning.”
The nomogram, which has been deployed as a freely available online risk calculator at https://riskcalc.org/COVID19/ , was developed using data from nearly 12,000 patients enrolled in Cleveland Clinic’s COVID-19 Registry, which includes all individuals tested at Cleveland Clinic for the disease, not just those that test positive.
Data scientists, including co-author on the study Michael Kattan, Ph.D., chair of Lerner Research Institute’s Department of Quantitative Health Sciences, used statistical algorithms to transform data from registry patients’ electronic medical records into the first-of-its-kind nomogram.
This study revealed several novel insights into disease risk, including:
“Our findings corroborated several risk factors already reported in existing literature – including that being male and of advancing age both increase the likelihood of testing positive for COVID-19 – but we also put forth some new associations,” said Dr. Jehi. “Further validation and research are needed into these initial insights but these correlations are extremely intriguing.”
In a previous network medicine study led by Lerner Research Institute scientists, 16 drugs (including melatonin, carvedilol and paroxetine) and three drug combinations were identified as candidates for repurposing as potential COVID-19 treatments. While these findings suggest an association between taking these medications and reduced risk of testing positive for COVID-19, additional studies are needed to assess how these drugs may affect disease progression.
“The data suggest some interesting correlations but do not confer cause and effect,” said Kattan. “For example, our data do not prove that melatonin reduces your risk of testing positive for COVID-19. There may be something else about patients who take melatonin that is indeed responsible for their apparent reduced risk, and we don’t know what that is. Consumers should not change anything about their behavior based on our findings.”
The nomogram, developed using data from patients tested at Cleveland Clinic for COVID-19 before April 2, 2020, showed good performance and reliability when used in a different geographic region (Florida) and over time (patients tested after April 2, 2020). This suggests that the patterns and predictors identified in the model are consistent across regions and communities and can be potentially adopted for clinical practice in healthcare systems across the country.
“This nomogram will bring precision medicine to the COVID-19 pandemic, helping to enable researchers and physicians to predict an individual’s risk of testing positive,” said Kattan. “Additionally, while testing solutions continue to be needed, it is so important to make sure we are responsibly and optimally dispatching our resources - including clinical personnel, personal protective equipment and hospital beds. Our risk prediction model stands to greatly assist hospital systems in this planning.”
The COVID-19 research registry, which now has data from more than 23,000 patients, is being used to inform a variety of studies. Researchers from across the Cleveland Clinic enterprise are using the dynamic registry data in more than 140 COVID-19-related research projects in areas such as cancer, pediatrics and intensive care.
Cleveland Clinic is a nonprofit multispecialty academic medical center that integrates clinical and hospital care with research and education. Located in Cleveland, Ohio, it was founded in 1921 by four renowned physicians with a vision of providing outstanding patient care based upon the principles of cooperation, compassion and innovation. Cleveland Clinic has pioneered many medical breakthroughs, including coronary artery bypass surgery and the first face transplant in the United States. Cleveland Clinic is consistently recognized in the U.S. and throughout the world for its expertise and care. Among Cleveland Clinic’s 82,600 employees worldwide are more than 5,786 salaried physicians and researchers, and 20,700 registered nurses and advanced practice providers, representing 140 medical specialties and subspecialties. Cleveland Clinic is a 6,728-bed health system that includes a 173-acre main campus near downtown Cleveland, 23 hospitals, 280 outpatient facilities, including locations in northeast Ohio; Florida; Las Vegas, Nevada; Toronto, Canada; Abu Dhabi, UAE; and London, England. In 2024, there were 15.7 million outpatient encounters, 333,000 hospital admissions and observations, and 320,000 surgeries and procedures throughout Cleveland Clinic’s health system. Patients came for treatment from every state and 112 countries. Visit us at clevelandclinic.org. Follow us at x.com/CleClinicNews. News and resources are available at newsroom.clevelandclinic.org.
Editor’s Note: Cleveland Clinic News Service is available to provide broadcast-quality interviews and B-roll upon request.