Figure includes financial assistance, outreach programs, education, research
Cleveland Clinic News Service | 216.444.0141
We’re available to shoot custom interviews & b-roll for media outlets upon request.
CCNS health and medical content is consumer-friendly, professional broadcast quality (available in HD), and available to media outlets each day.

In 2017 Cleveland Clinic provided $906.5 million in community benefit – including financial assistance, Medicaid shortfall, subsidized health services, outreach programs, education and research – the highest level in our reporting history.
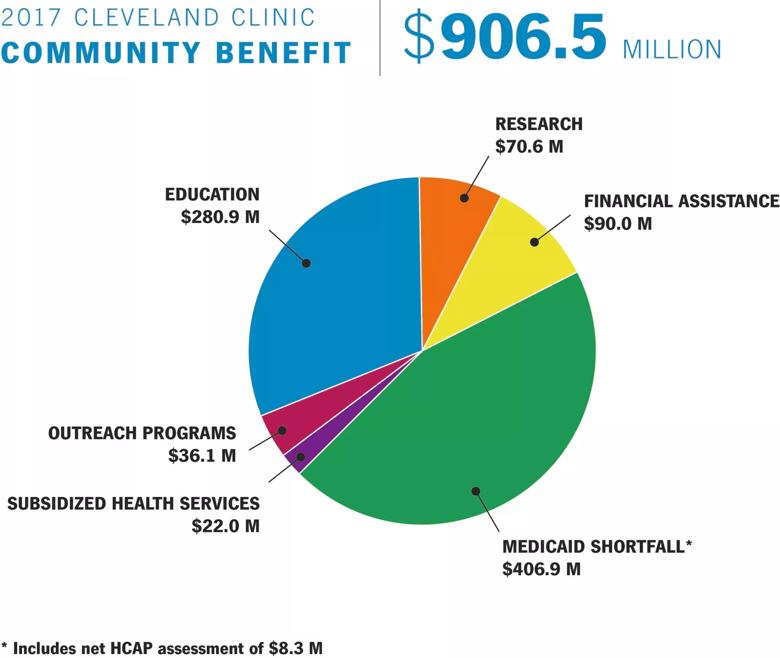
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/75c857d2-78ee-4be5-8fe5-17730264f2af/Comm-benefit-2017-11-30-18-scaled_jpg)
The total – a 5 percent increase over 2016 – includes all health system operations in Ohio, Nevada and Florida.
“Cleveland Clinic is committed to creating healthier communities,” said Tom Mihaljevic, M.D., CEO and president of Cleveland Clinic. “Our community benefit is far-reaching, including healthcare access for everyone in our communities; the education of the next generation of healthcare professionals; free prevention and screening programs; and medical research that leads to advanced treatments and cures.”
Cleveland Clinic calculates community benefit conforming to the IRS Form 990 reporting guidelines, which include activities or programs that improve access to health services, enhance public health, advance general knowledge and relieve government burden. The primary categories for assessing community benefit include financial assistance, Medicaid shortfall, subsidized health services, outreach programs, education and research:
Financial assistance increased 4 percent over 2016 and includes free or discounted care provided to patients who are unable to pay some or all of their bills. Cleveland Clinic’s financial assistance policy provides free or discounted care to patients with incomes up to 400 percent of the federal poverty level.
Medicaid provides government-funded healthcare coverage for low-income families and individuals. However, in many states, including Ohio, Medicaid payments do not sufficiently cover the costs of treating Medicaid beneficiaries. In 2017, Cleveland Clinic’s Medicaid costs were $406.9 million – a 7.1 percent increase over 2016 – including an $8.3 million net contribution to Ohio’s Hospital Care Assurance Program (HCAP). (The 2016 Medicaid shortfall has been revised upward to properly reflect costs which were previously understated.)
These are clinical services provided to meet the needs of the community despite creating a financial loss for the hospital system, such as behavioral health, obstetric and chronic disease management, among others. The 2017 total represents a 12.4 percent increase from 2016.
Costs for training health professionals – medical residents, fellows, nurses and allied health professionals – increased 3.2 percent from 2016 to 2017, while research expenses increased 10.3 percent.
Cleveland Clinic’s outreach programs align with the local needs identified in the hospitals’ Community Health Needs Assessments, with an emphasis on prevention, wellness and chronic disease management. Examples include:
As a nonprofit hospital system, Cleveland Clinic is a community asset with no owners, investors or stockholders. Any and all extra funds from operations are invested back into the health system to support patient care, research, education, and long-standing charitable efforts.
Read or download the entire report here.
About Cleveland Clinic
Cleveland Clinic is a nonprofit multispecialty academic medical center that integrates clinical and hospital care with research and education. Located in Cleveland, Ohio, it was founded in 1921 by four renowned physicians with a vision of providing outstanding patient care based upon the principles of cooperation, compassion and innovation. Cleveland Clinic has pioneered many medical breakthroughs, including coronary artery bypass surgery and the first face transplant in the United States. U.S. News & World Report consistently names Cleveland Clinic as one of the nation’s best hospitals in its annual “America’s Best Hospitals” survey. Among Cleveland Clinic’s 52,000 employees are more than 3,600 full-time salaried physicians and researchers and 14,000 nurses, representing 140 medical specialties and subspecialties. Cleveland Clinic’s health system includes a 165-acre main campus near downtown Cleveland, 11 regional hospitals, more than 150 northern Ohio outpatient locations – including 18 full-service family health centers and three health and wellness centers – and locations in Weston, Fla.; Las Vegas, Nev.; Toronto, Canada; Abu Dhabi, UAE; and London, England. In 2017, there were 7.6 million outpatient visits, 229,000 hospital admissions and 207,000 surgical cases throughout Cleveland Clinic’s health system. Patients came for treatment from every state and 185 countries. Visit us at clevelandclinic.org. Follow us at twitter.com/ClevelandClinic. News and resources available at newsroom.clevelandclinic.org.