
By Adam Myers, M.D., MHCM, FACHE
Chief of Population Health and chair of Cleveland Clinic Community Care

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6ead81af-bf8d-45c2-aa47-ecbb983d8933/Myers_Adam_709412_jpg)
Adam Myers, M.D.
Research clearly shows that we underutilize advanced directives in the United States. It also shows that patients often don’t feel informed and equipped to make even the everyday healthcare decisions we face, let alone those surrounding end-of-life options.
My mother died last year. It was both sudden and unexpected. One day she was the cantankerous mother I knew and loved, the next minute she faced a grim prognosis from acute leukemia. Her first symptoms appeared only seven days before she died.
Once the diagnosis was certain, the cancer team leader came to discuss treatment options. Those options focused primarily on possible extension of life. Very little was said about the other side of the equation. What would life be like during treatment?
For years, our cultural expectation is that we receive healthcare. I would argue that we must participate in our own healthcare. Otherwise, some obvious solutions to health problems can be overlooked and unaddressed. Additionally, your preferences for care are much less likely to be honored if you do not express them.
Fortunately, my family is proactive about discussing end-of- life situations. We embrace advanced directives as a good way to address potential end-of-life options. We realize that it is easier to do so calmly when you are not actually facing an end-of-life situation and that doing so is a true service to those who may have to make those decisions on our behalf. Additionally, none of us – thanks to our mother — are shy about asking difficult questions. With support from us, my mom asked a very simple yet important question, “How will I feel during treatment?”
She had already accepted that she would ultimately die from this aggressive cancer. While possibly extending her time was desirable, she wanted to know what would be involved. Would she need a port to receive medications? How often would she need treatment? How would it feel? How often would the treatment involve leaving home? What could go wrong?
With family support, she was able get those answers and realized that palliative care was the option she wanted. The cancer team still encouraged her to enter treatment, however my mom stuck to her plan. She died peacefully four days later in the way she chose.
Oftentimes, patients and their loved ones rely too heavily on the knowledge and opinions of their medical practitioners when mapping out a treatment plan. And that’s understandable, given the vast training physicians and nurses undergo so they can effectively treat their patients.
But patients – as well as those who love them – do well to actively participate in the decision-making process, whether for minor conditions or significant health crises. Both medical and personal perspectives are vital when considering any course of treatment. Such shared decision-making leads to better decisions.
Patients are well served to take a more vigorous role in their own health, especially when they’re speaking directly to their care team.
Not sure what to say? Here are a few questions and topics to get you started.
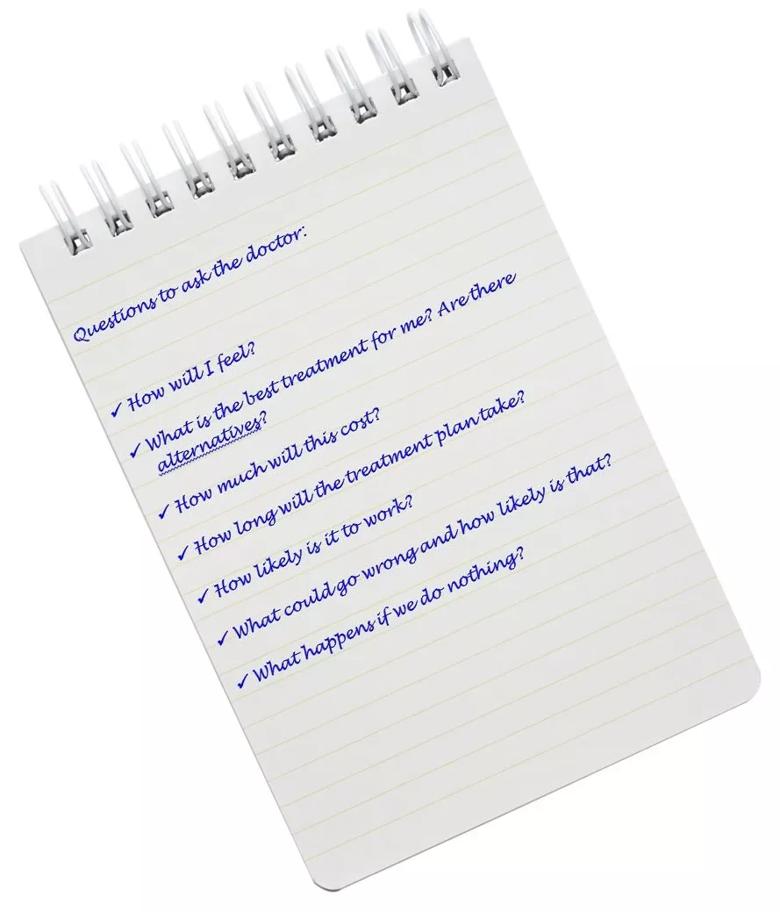
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e251afd-a6d6-4310-89ea-5a758c2c4648/qs-for-dr3_jpg)
I always encourage patients to ask about the logistics of a treatment plan, too. Questions like:
One more piece of advice: Be prepared. Some of that starts with advanced directives. Addressing those options before you face actual end-of -life reality makes for better decisions.
Unless you’re making a sudden trip to the emergency department, you will likely have time before a doctor’s visit to think about your medical condition. You can then provide all the information needed for your care team to make an accurate diagnosis and attain effective treatment. That includes making a list of your existing prescriptions, what you think might be impacting your health and, of course, the specific questions for which you need answers.
Your list may hold the key to a healthier, happier life.