Updated October 19, 2020

Following guidelines from the Centers for Disease Control and Prevention (CDC), this document has been updated as of October 19, 2020. For the latest information about COVID-19 including how it spreads, prevention and treatment, and symptoms, visit the CDC’s website.
A: COVID-19 is a virus strain primarily spread through respiratory droplets. That means to become infected, you generally must be within six feet of someone who is contagious and come into contact with these droplets. It may be possible to get COVID-19 by touching a surface or object that has the virus on it and then touching your mouth, nose, or possibly your eyes. People with COVID-19 have had a wide range of symptoms ranging from mild symptoms to severe illness.
Symptoms of COVID-19 may appear within two to 14 days after exposure and include:
This list does not include all possible symptoms. Children have similar symptoms to adults and generally have mild illness.
A: Practice the following:

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6e2e10d5-4bc6-4cd4-ba64-4f8a282ee860/Prevention-graphic_cloth-mask-update_04_07_20_jpg)
A: Unfortunately, there is not yet a vaccine that can prevent COVID-19, so we cannot prevent the disease.
The coronavirus that causes COVID-19 is new, so we are just learning how it impacts specific groups of high-risk people. But, those who are thought to be most susceptible to serious complications of COVID-19 include people who:
But there are things you can do to minimize your risk if you have a weakened immune system or are immunocompromised.
Find out what steps you should take if you’re considered high risk
A: African Americans are more likely to acquire and die from complications of the COVID-19 virus because Blacks suffer from higher rates of chronic medical conditions like diabetes and obesity, high blood pressure, heart and kidney disease and asthma. All of these lower the immune system and the ability to fight off viruses. Additionally, lifestyle factors like being an essential worker and even using public transportation increase the risk of getting COVID-19.
A: During this unprecedented time, Cleveland Clinic has taken a number of steps to help limit the spread of COVID-19 and ensure our hospitals are safe for caregivers and patients. This includes providing appropriate personal protective equipment for caregivers, offering masks to patients, visitors, caregivers and vendors, limiting access into our facilities, limiting visitation, canceling public events and checking the temperature of everyone who enters our doors.
A: The safety of our patients and caregivers remains our top priority. We want to assure patients that our Cleveland Clinic facilities are safe for them to receive care.
We have taken steps to increase safety by:
If you’re unsure about keeping your appointment, contact your physician’s office to see if other options are available.
A: As we learn more about COVID-19 and its transmission, we are adapting our practices in order to provide the safest care to our patients and protect our caregivers. In alignment with guidelines from the CDC and direction from our state and local governments, we are requiring all caregivers in all our locations to wear face masks while inside our facilities.
Face masks are required for patients at all routine appointments and procedures (without a hospital stay), Emergency Department patients, and permitted visitors. Face masks are strongly encouraged for patients admitted to the hospital, unless they have a health or behavioral condition that prevents them from wearing one. Patients and permitted visitors will be given a mask to wear the entire time they are in our facilities. They may choose to bring their own masks from home. Wearing a mask is not only an effort to protect yourself, but also to help protect others.
A: Please bring your appointment reminder with you (email, MyChart or text message). When entering any Cleveland Clinic location, you and any permitted visitors (see visitor restrictions) will be screened for potential COVID-19 symptoms, including a temperature scan. In some locations, we use no-contact, hand-held thermal scanners. In other places, we use a thermal imaging system you walk through and might not even notice. You’ll be asked to sanitize your hands.
For a routine appointment or procedure (without a hospital stay, and Emergency Department visits, patients are required to wear a mask while inside our facilities, unless they have a health or behavioral condition that prevents them from wearing one. Patients admitted to the hospital are strongly encouraged to wear a mask while inside our Ohio and Florida facilities. Masks from home may be worn, or masks will be provided at entrances.
A: We have taken a number of steps to ensure our facilities are safe to protect our caregivers and patients and help limit the spread of COVID-19. As the pandemic continues, we designed visitation policy that will adjust as COVID fluctuates within our states. Please see our current visitor restrictions.
A: Yes, all Cleveland Clinic emergency departments remain open for care. We encourage the public to seek immediate medical attention for symptoms that suggest serious medical emergencies, such as stroke or heart attack. All patients coming to our emergency departments are screened for COVID-19 symptoms and are required to wear a mask, unless they have a health or behavioral condition that prevents them from wearing one. This is to help maintain the health and safety of our patients and caregivers and prevent the spread of the virus. Any patients with COVID-19 symptoms are taken to a designated area within the emergency department for care.
A. We’re using four new, statewide visitation levels — yellow, orange, red and purple — to protect our patients and caregivers and limit the spread of COVID-19. The visitation levels are based on data about how COVID-19 is spreading, including state and county public health information. If you are visiting a COVID-19 positive patient, you must wear provided personal protective equipment (PPE). Even when you can’t visit in person, we encourage you to stay connected virtually.
These guidelines are being put in place for the safety of our patients, caregivers and community. Thank you for your understanding.
Please note: All visitors must wear a mask, have their temperature taken and sanitize their hands. Visitation guidelines are subject to change if safe physical distancing isn’t possible.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1902be35-4981-4d93-9d6c-ac57d07aec5b/Visitation-levels-9_30_jpg)
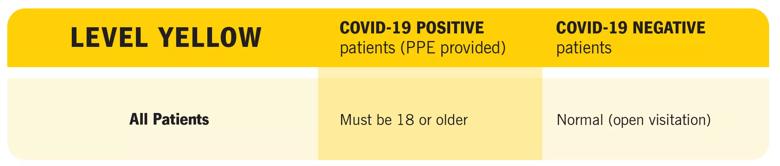
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f6bb2889-3e62-4296-a646-440e2f7bb8c3/Yellow-Level_jpg)
Please note: Patients must follow all social distancing and masking guidelines.
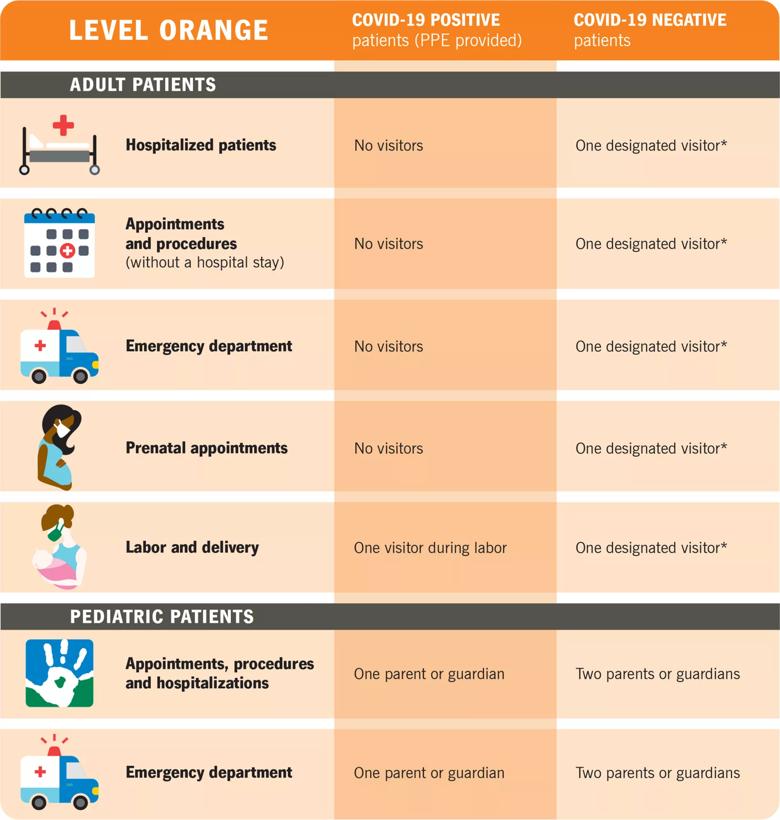
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b3feff95-cd28-470e-98fc-b98f18f79086/Orange-Level-2-scaled_jpg)
Please note: A patient’s care team may make compassionate exceptions, when appropriate.
*Patients may choose one individual (18 or older) to be their designated visitor. That designated visitor may visit each day during the patient’s hospital stay.
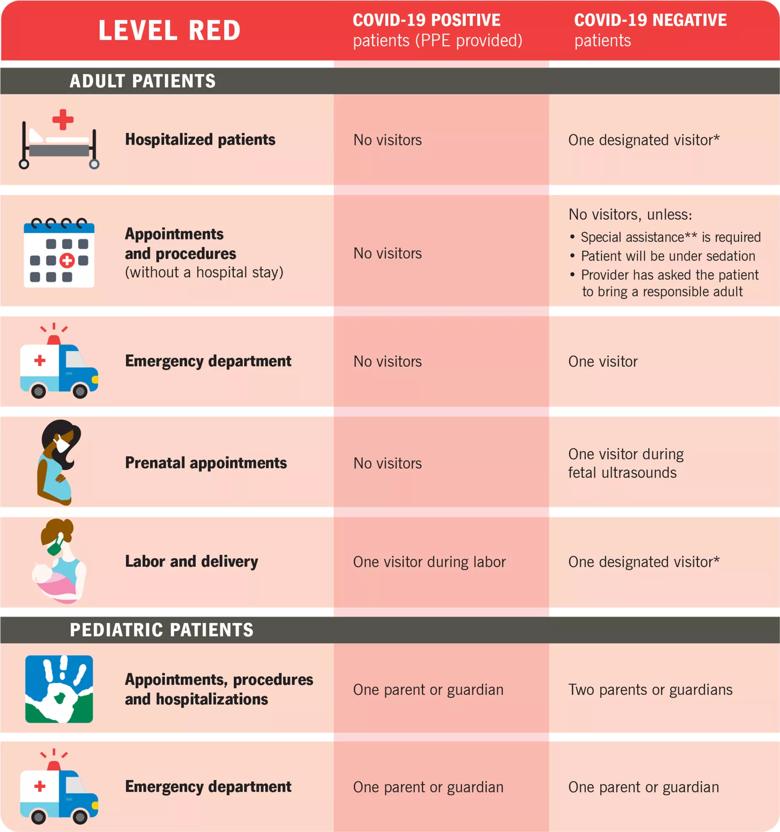
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7326c7d3-1473-4b37-97b4-0974d44bd0f7/Red-Level-2-scaled_jpg)
Please note: A patient’s care team may make compassionate exceptions, when appropriate.
*Patients may choose one individual (18 or older) to be their designated visitor. That designated visitor may visit each day during the patient’s hospital stay.
**Special assistance is any circumstance where a patient’s care team determines that a visitor is critical to physical or emotional care.
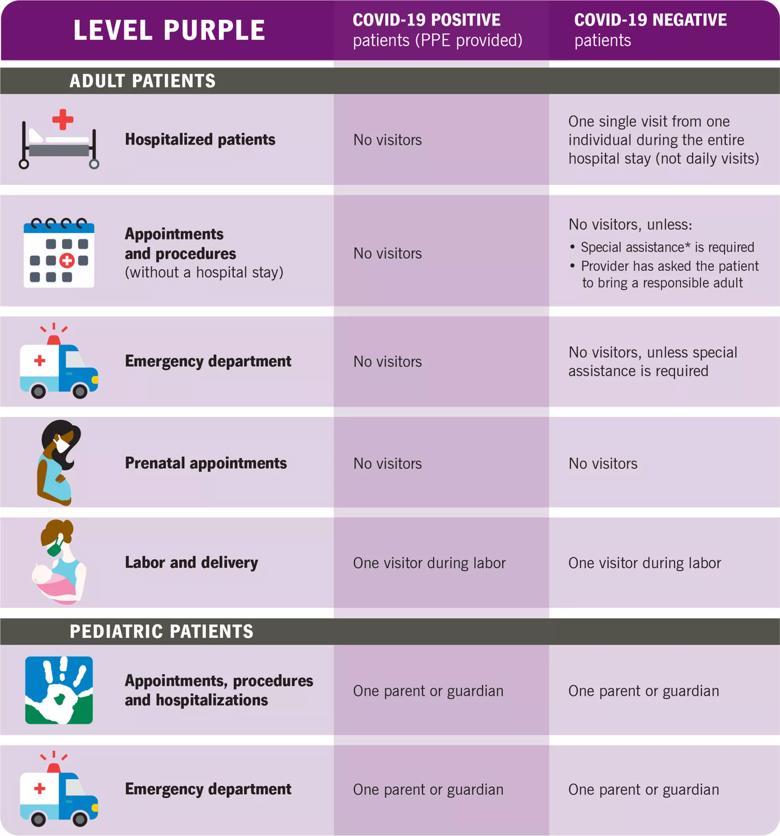
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/85828689-a1bc-467c-b7c8-fecad2adae54/Purple-Level-2-scaled_jpg)
Please note: A patient’s care team may make compassionate exceptions, when appropriate.
*Special assistance is any circumstance where a patient’s care team determines that a visitor is critical to physical or emotional care.
Visitor Guidelines for Locations Other Than Ohio and Florida:
For All Permitted Visitors:
A: Yes. Cleveland Clinic launched a free COVID-19 screening tool to find out your risk level based on symptoms and travel.
Follow these steps:
A: Cleveland Clinic is providing drive-up and on-site testing for patients suspected of having COVID-19. Patients will need to be evaluated by a clinician using Cleveland Clinic Express Care Online or in-person, and will need a Cleveland Clinic electronic doctor’s order to be tested.
These patients will continue to be tested at Cleveland Clinic testing sites with a Cleveland Clinic physician’s order.
All patients with scheduled surgeries or procedures that will take place in an ambulatory surgery center or operating room will be tested for COVID-19 before their surgery or procedure. They will be given a date and time for a testing appointment. We have several testing locations throughout northeast Ohio, and will work with the patient to schedule an appointment at a location most convenient for them.
Testing is open 11 a.m. – 5 p.m., seven days a week. A Cleveland Clinic electronic provider’s order is required for COVID-19 testing.
It will be important to practice the following precautions to help prevent COVID-19 until the test result comes back and until the time of surgery:
A: One way we maintain a safe environment for our patients and caregivers is by requiring patients to undergo COVID-19 testing within three days prior to any surgery or procedure in a Cleveland Clinic operating room, ambulatory surgery center and select locations.
Recently published data in The Lancet supports our pre-operative testing requirement. The study found that asymptomatic patients with COVID-19 were at higher risk of post-operative complications. By requiring patients to complete pre-operative testing, we help protect our patients and caregivers.
A: All patients with scheduled surgeries or procedures taking place in a Cleveland Clinic ambulatory surgery center or operating room will be tested for COVID-19 within three days, or 72 hours, prior to their surgery or procedure date. When a surgery or procedure is scheduled, a COVID-19 test will also be ordered.
We have several testing locations, throughout Northeast Ohio and Florida, designated for patients who have an upcoming surgery or procedure. An appointment for the COVID-19 test will be scheduled at a location and time most convenient for the patient.
A: Ohio:
Testing Locations:
On-site testing is located in the garage of the W.O. Walker Building at Cleveland Clinic’s main campus, at Akron General Akron Health Center and at Cleveland Clinic’s Akron General Health and Wellness Center in Green.
Please Note: A Cleveland Clinic electronic provider’s order is required for COVID-19 testing.
Directions to Testing Locations:
W.O. Walker Building
10524 Euclid Ave.
Cleveland, OH 44195
Patients should enter the garage from E. 105th St.
Testing hours:
Daily, 10 a.m. – 5 p.m.
Akron General Akron Health Center
676 South Broadway St.
Akron , Ohio 44311
Testing hours:
Monday – Friday, 9 a.m. – 5 p.m.
Akron General Health and Wellness Center, Green
1940 Town Park Blvd.
Uniontown, OH 44685
Testing hours:
6 days a week (closed Thursdays), 9 a.m. – 5 p.m.
Florida:
Cleveland Clinic is providing drive-through COVID-19 testing for patients in Florida. Individuals must have an appointment in order to be tested.
Testing Locations
On-site testing is located at Weston Hospital, Martin North Hospital in Stuart, Martin Health at St. Lucie West and Indian River Hospital in Vero Beach.
Please Note: An appointment from Cleveland Clinic Florida is required for COVID-19 testing.
What is the process for getting tested?
Only patients with an appointment will be seen at the drive-through testing. Patients should start by calling our nurse triage hotline to schedule their appointment for testing:
The caller will be screened by a nurse who will determine if they meet criteria for testing.
Patients who meet the criteria for COVID-19 testing will be given an appointment and directed to the testing location.
At Cleveland Clinic Weston, anyone over the age of 16 who has COVID-19 symptoms, as defined by the CDC, is eligible for testing.
At Cleveland Clinic Martin Health and Cleveland Clinic Indian River, anyone over the age of 5 who has COVID-19 symptoms, as defined by the CDC, is eligible for testing.
Directions and Hours for Testing Locations:
Weston Hospital
First Floor
2950 Cleveland Clinic Blvd.
Weston, Florida 33331
Testing Hours:
Monday – Friday, 8 a.m. – 5 p.m.
Martin North Hospital
200 SE Hospital Ave.
Stuart, Florida 34994
Testing Hours:
Monday – Friday, 8:30 a.m. – 3:30 p.m.
Saturday – Sunday, 9 a.m. 1 p.m.
Martin Health at St. Lucie West
1095 NW St. Lucie West Blvd.
Port St. Lucie, Florida 34986
Testing Hours:
Monday – Friday, 8:30 a.m. – 3:30 p.m.
Saturday – Sunday, 9 a.m. – 1 p.m.
Indian River Hospital
Patient Pavilion
1000 36th Street
Vero Beach, Florida 32960
Testing Hours:
Monday – Friday 7 a.m. – 3 p.m.
A: For patients in the hospital, and those tested in our Emergency Departments who are considered very ill or at risk, results are available on average within 24 hours.
For patients being tested at our drive-thru facility, results are available on average within a few days. Patients are asked to remain at home until their test results are released. Once processed, COVID-19 test results will now be available immediately in a patient’s MyChart, our secure online health management tool.
A: Based on your symptoms, do the following:
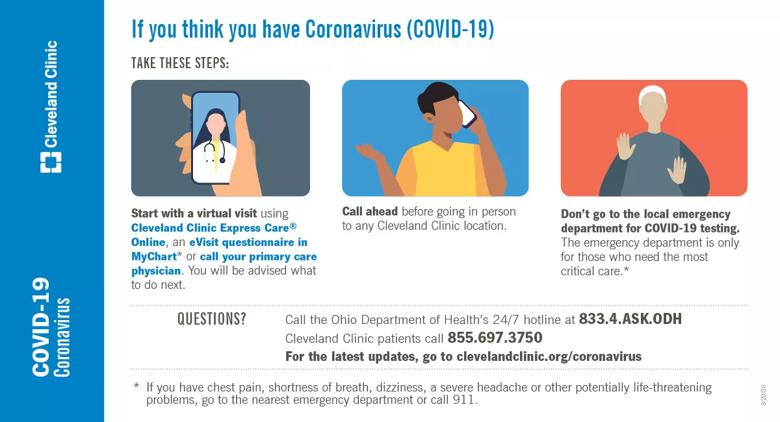
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a431bf18-290f-461c-a640-fe46a6dcc43b/20-CCC-1869334-TakeTheseSteps_Infog-FB-Twitter_jpg)
Centers for Disease Control and Prevention
Southern Nevada Health District
About Cleveland Clinic
Cleveland Clinicis a nonprofit multispecialty academic medical center that integrates clinical and hospital care with research and education. Located in Cleveland, Ohio, it was founded in 1921 by four renowned physicians with a vision of providing outstanding patient care based upon the principles of cooperation, compassion and innovation. Cleveland Clinic has pioneered many medical breakthroughs, including coronary artery bypass surgery and the first face transplant in the United States. U.S. News & World Report consistently names Cleveland Clinic as one of the nation’s best hospitals in its annual “America’s Best Hospitals” survey. Among Cleveland Clinic’s 67,554 employees worldwide are more than 4,520 salaried physicians and researchers, and 17,000 registered nurses and advanced practice providers, representing 140 medical specialties and subspecialties. Cleveland Clinic is a 6,026-bed health system that includes a 165-acre main campus near downtown Cleveland, 18 hospitals, more than 220 outpatient facilities, and locations in southeast Florida; Las Vegas, Nevada; Toronto, Canada; Abu Dhabi, UAE; and London, England. In 2019, there were 9.8 million total outpatient visits, 309,000 hospital admissions and observations, and 255,000 surgical cases throughout Cleveland Clinic’s health system. Patients came for treatment from every state and 185 countries. Visit us at clevelandclinic.org. Follow us at twitter.com/CCforMedia and twitter.com/ClevelandClinic. News and resources available at newsroom.clevelandclinic.org.
Editor’s Note: Cleveland Clinic News Service is available to provide broadcast-quality interviews and B-roll upon request.